All about Vaccine: A Conversation with Researcher Dr. Ines Atmosukarto

Devi: Hi everyone! I hope you’re all in good health. Welcome to Magdalene’s Mind! I’m Devi Asmarani
Hera: And I’m Hera Diani. We’re still actually on bonus episode because Magdalene’s Mind is still vacuum while we are producing other podcasts.
Devi: That’s right. This is a special episode for a special day: the International Women’s Day. For feminists this is like our major holiday. On this day we celebrate the diversity of women’s experiences, challenge norms and practices that are discriminative on the basis of gender, and push for gender equality and women’s empowerment.
Hera: That is why today Magdalene’s Mind is back on air with a very relevant theme for this day and within the context of the COVID-19 pandemic. I’m actually really excited to be talking on Magdalene’s Mind again.
Devi: I know, I really miss Magdalene’s Mind. It’s been a year since the last season of the series ended, although we do have some bonus episodes. But we did have to take a break while we produced a couple of important podcasts: one of them is about women’s leadership – How Women Lead – while the other one is about media and gender, the FTW Media. So you can check these two podcasts on any of the platforms that you use.
Anyhow, back to the topic of the episode. You want to talk about it, Her?
Hera: So, just like Devi was saying, it’s been a year since the pandemic started in Indonesia and in that span of time one of the focuses was directed in developing the COVID-19 vaccine in the shortest time possible. In Indonesia, the vaccine has been distributed since the beginning of the year.
Devi: Yep, however, there are still so much information swirling around on vaccine, and some of them can be confusing, and even resulting in hoax. That is why today we are talking to scientist from Indonesia who focuses on vaccine innovation and development.
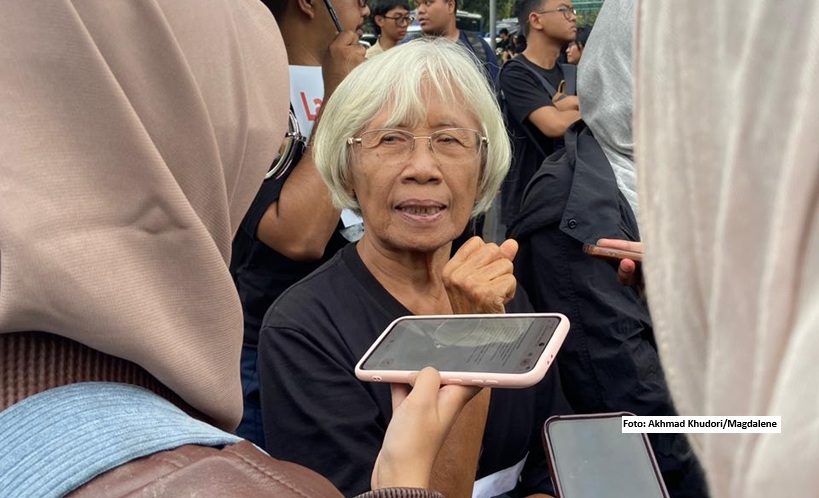
Hera: Yes, we have invited Dr Ines Atmosukarto, CEO of Lipotek Pty, Ltd, di Australia, which develops technology or design vaccines, not just for Corona virus.
Devi: We talked a lot about different things, from the pandemic, to people who are sceptical of vaccines, to challenges that women in science face. Dr. Ines is one of the few women who build a career in scientific research. According to a 2015 UNESCO research, globally, only 28 percent of researchers are women, despite the fact that there are equal number of men and women who graduated with undergrad and graduate degrees in STEM.
Hera: So, stay tune after this message, all!
Also read: The Courageous Pioneer
COMMERCIAL BREAK
Back to Magdalene’s Mind with Dr. Ines Atmosukarto.
Dr Ines is one of the five women in the world to receive UNESCO’s L’Oreal Fellowship for Women in Science in 2004. Currently, her work focuses on the development of vaccines.
Thank you for joining Ines. Jumping straight in, we would like to know more about what got you interested in becoming a scientist?
Ines: My interest in science actually developed from my family. My father, mother, grandfather from my mom, they were all scientists. My dad was an engineer, my mother was an expert in nuclear physics. My maternal uncle is the head of a unit of nuclear physicians in Romania, and so on. We all came from science background. So from childhood we were taught about facts, science. So, I think that’s probably how I ended up gaining an interest in the field of science.
Were you in Indonesia or outside of Indonesia at the time?
Ines: I’ve attended many schools actually and therefore experienced different school systems. In elementary school I was French school, because my dad worked as an engineer in Algeria. In 7th grade my parents decided to move to Indonesia, where I graduated from high school. Before that we never set foot in Indonesia, didn’t speak Indonesian, but then we continued our education until we finished high school in Indonesia. Following this, I received a scholarship to Adelaide, Australia to continue my study as an undergraduate in 1992.
It is noteworthy that the participation of women in the world of science and STEM remains considerably low even today – according to a UNESCO study, less than 30% of the world’s researchers are women. Why do you think this is the case?
Ines: This is an unfortunate truth, common to countries across the world. I think it comes down to the notion that it is the nature of women to assume maternal roles. Because women bear children and have to take care of them at least in the first few years, in the end it becomes burden for women in pursuing career in comparison to men.
Do you think there should be a policy for female scientists to deal with this issue?
Ines: While I think it is necessary, however it is also not easy as there are a lot of factors that need to be accounted for – such as childcare, a flexible work environment, etc. – that come into play. In the end gender diversity is very important.
This is related to the participation of women in the world of STEM. You have helped create fellowship programs for young Indonesian women in the field of science. Can you tell us a bit about this and what are the challenges that you’ve faced?
Ines: In 2004, after receiving the international fellowship, L’Oreal Indonesia took the initiative to start national fellowship programs to support young female researchers and also programs to stimulate an interest in the world of science to young females in elementary and middle school as a way to introduce this field to them at an early age. The goal was to break the stigma and highlight that women too can have careers as scientists and researchers. There were many challenges, one of which was funding. Both international and national branches of L’Oreal really got on board. Another challenge was trying to break the stigma. We want to create an environment where the youth feel empowered to discuss issues with their mentors.
In this pandemic, words like “vaccines” and “immunology” have become household terms. As someone who has worked at length on vaccine development technology, could you share with us the process of creating vaccines? And how long would it take until the vaccine is ready to use?
Ines: From the perspective of a researcher in the field of vaccines, when looking for support and cooperation from pharmaceutical companies, vaccines are not considered as an interesting product. Firstly, it’s because basically, vaccines are always designed to be sold cheap so that most, if not all, people can afford it. Next, vaccines are preventive products where a single use by an individual is expected to cure them. From a business model perspective, it’s actually not a very good product. Because I work in a biotech startup, one of the biggest challenges is to convince investors that investing in vaccines is important. In this case, the pandemic is helping as it shows that vaccines are proven to be one way out of this pandemic. The development process of a vaccine actually takes a long time – traditionally, about 10 to 15 years. The vaccine for this pandemic actually holds a record for fastest development time, about 12 months. This was possible due to the massive funding received from various parties, which fastens development time as well as testing phases.
A lot of people are still confused about how vaccines work, why must we take needle shots and how they prevent the virus. Can you give us a simplified explanation?
Ines: Vaccines are a tool to teach your body to understand a virus. So that if our body is exposed to the virus, it can prevent the virus from infecting our body quicker. Basically, there are 3 important cells in our immune system. The first one is called the dendritic cell; it acts as the patrol in our body looking for foreign objects. Once it has found a foreign object, essentially it will “consume” the said foreign object and processes it. This is its way to teach the other cells about the foreign object (in this case, a virus). The other cells are the B cell and the T cell. With the help of the processed information, the B cell creates a specific antibody to act against the virus. In the case where the antibody doesn’t work against the virus, the T cell acts as the backup plan. It looks around for infected cells caused by the virus that slipped away from the antibody and eliminates them. What a vaccine does is that it allows these cells to identify the virus without risking our bodies to be exposed to the virus first. That’s the beauty of the vaccine. It is normal for your body to feel uncomfortable after a vaccination shot. Slight fevers and the likes show that your immune system is benefitting from the vaccine. Honestly, I’d be more concerned about the people who say they don’t feel anything after a vaccination shot because vaccines are supposed to stimulate our immune systems, and when it’s stimulated, we’re sure to feel something in our body. So that’s how a vaccine works, a master educator for our bodies to create relevant antibodies.
You mentioned earlier that it doesn’t take 10 to 15 years anymore due to more people being involved. Some people might think “was it rushed?”. They might still be doubtful and scared of the vaccine, how would we know that the vaccine is safe and effective?
Ines: I understand that people might think it’s odd how fast the development is going. However, the development process is also very transparent. There is a lot of information out there about this, especially due to how fast information is communicated in today’s era. This transparency gives me confidence in the safety of the vaccine. Also, all vaccines used are evaluated by local authorities (BPOM, FDA, EMA). It is their job to evaluate all data given to them from the first to the last phase of testing. The researchers in said authorities will reanalyze the data given to consider whether they agree with the conclusion made by the developer researcher for the vaccine itself. There was a case in America regarding the Pfizer vaccine, after millions were vaccinated, a few hundred reported allergic reactions. This was immediately reported and although the risk was low, they prepared for it. Now, after taking the vaccine we are asked to wait 30 minutes to ensure no allergic reactions occur. If it does occur, personnel are on standby and ready to take care of it.
As we know, there are people who have low confidence in vaccines, especially when it comes to children. What are the larger implications of this?
Ines: Unfortunately, people can afford to be skeptical of vaccines because they never see for themselves the impact of the disease that can be prevented by vaccine on someone. For example, me, I’ve never met someone who suffered from polio. But my parents’ generation, they almost certainly know someone who had polio when they were young and they could see for themselves the impact of polio – including being disabled. Because vaccines is so efficient in preventing diseases, it actually becomes its worst enemy. Because the particular diseases have been eradicated, so people say, ‘It’s okay to catch the disease.’ They do not take into consideration long-term effect of the disease. It’s just like COVID-19, some people are saying, ‘Ah, it’s only COVID-19. No big deal.’ You don’t know the long term effect, because this is a new disease. Even if we have recovered from it, or did not have symptoms, it doesn’t mean that nothing happened in our body. So getting vaccinated lowers all the risks. But it’s hard to counter people who have this mindset. In Australia, most of them live in rich areas. They live in their comfort and secure bubble and they do not see what virus and infectious diseases do. They are actually a victim of their own bubble. And many would only realize the importance of getting vaccinated when their children contract the disease. So it’s our job for scientists to communicate this. But I think this needs to be taught from school because we know that teaching kids are esier than teaching adults.
You’re active on educating the public on vaccines and immunology using social media. Other researchers have also done the same thing. We want to ask you; how do scientists fight these circulating hoaxes regarding our situation?
Ines: If only I knew. Honestly, it’s difficult and I’m still learning. I resisted social media for a long time and did not even have any presence on it until end of last year. At the end of last year, I followed the discourse in Indonesia surrounding COVID-19, diseases, vaccines and realized that we need more people to voice latest, scientific information in an easy-to-understand manner. Fighting with facts and data can even be ineffective in certain cases, as there can be those who have already believed other facts and sources, and it’s difficult to change their beliefs. What I’m trying now, is to understand why they believe these claims, so that we can start a discussion to try to change their stance on this matter, in a polite manner of course. Directly telling them that they are wrong is obviously ineffective. We need to continue evidence-based discussions in parallel, so people can find our point of views as well. I try to monitor the issues that are being discussed around hesitancy. The challenge is figuring out how to change their stance without putting the focus on them. I have learned from my kid, who is 22 years old, studying public health, and has more experience in social media. As a scientist, we also have to be humble. We do not know everything. We can be wrong. We have to learn from social scientists. We must talk to anthropologists or other social scientists to find ways [to address this].
This might be the last question. Now COVID-19 vaccines are being distributed in various countries, including in Indonesia. How can we make sure that this distribution of vaccines is fair and is easily accessible by everyone? Keeping in mind that Indonesia is an archipelago with remote areas, and in terms of equity, the gap is quite high. I read that in America, only about 5% of African Americans have received the vaccines so far. I believe there is a potential for a similar case to happen in Indonesia. What are your thoughts on this?
Ines: This is the thing that worries me the most: equity and equitability of the COVID-19 vaccines. Especially with Indonesia, there are many areas that are difficult to access – for example big cities vs. small ones. The government has to make sure that the vaccines are fairly distributed. That’s why they made the priority list from the beginning.
In the beginning, Indonesia’s priority was a bit different from other countries. This depends on the country’s social economy as well. In the USA, like you said, it could be the African Americans. In Australia, it’s the Aborigins that we have to pay attention to.
I think Indonesia is potentially having problems, as there are still some gaps in the vaccination program. For example, I was wondering, if the registration is done online, would this be accessible to some people?
It might be helpful for the public to monitor this and give feedback to the government, in a positive way. Criticism is not negative, as long as we do it with good intention. The government is also under huge pressure and has to take quick decisions. But with our feedback, the vaccination program can be managed better.
I also want to suggest that we pay attention to our community and help people around us to get the vaccines. For example, we can help elderlies by registering them, or by taking them to the hospital to get vaccinated.
Thank you for your time, Ines. It’s been a great conversation.